by Alisha Smith-Arthur
As I stood in line (safety distanced) to receive a COVID test before returning home to the US after a trip to Cote d’Ivoire in 2022, I was able to see and reflect upon the enduring legacy of the American public health diplomacy effort to fight the global pandemic of HIV. The testing site had the unmistakable dual-flag PEPFAR (The President’s Emergency Plan for AIDS Relief, announced by George W. Bush in 2003) logo outside, indicating that the testing equipment (and likely the training for the personnel inside) came via a PEPFAR project. I’ve seen similar stamps on rural labs and remote health posts across the countries I’ve worked in (as well as on the airport welcome signs of many a friendly health worker who has readily included me in their work), and it always serves to remind me of the common goals we are working towards in these health diplomacy projects.
The Impact of HIV
A generation ago, the world faced a major pandemic threat. A new virus, only somewhat understood by scientists and public health experts, was racing through communities worldwide with devastating effect. Startingly infectious, slow burning and fatal, the unfolding pandemic had been spreading for years without much attention and was now claiming victims at a shocking rate. Its mode of transmission—via bodily fluids, including from sex—tapped into social and cultural touchpoints, and science and punditry were quickly tangled between opinion, prejudice, and changing facts. Following the identification of the human immunodeficiency virus (HIV) and the syndrome that results if left untreated (AIDS) in the 1980s, fear-driven, politicized responses further marginalized affected communities and allowed the virus to spread.
The effects were devastating. As global systems began to catch up in the 1990s and better tallies were created, the numbers that emerged were appalling—at least three million people were estimated to have died in 2003 alone, and 1 in 5 adults in Sub-Saharan Africa were infected, with some countries facing infection rates of 40% or more. For those who lived and worked in Southern Africa, where the virus exploded, the daily impact of the pandemic will never be forgotten—in the young adults who seemed to disappear from day to day, the heart-breaking emergence of a growing generation of “AIDS orphans,” and the indelible images of coffin-sellers spreading their wares along the streets of too many villages and cities.
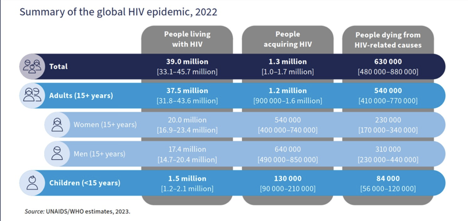
Infections were also expanding rapidly across the global, mostly in lower- and middle-income countries across eastern Europe, in Asia and the Pacific, in Latin America, and in disadvantaged and marginalized communities in western Europe and North America. By 2003, more than 40 million people globally were infected, people who would grow steadily sicker and eventually die, accelerating a world-wide tragedy that would cause immeasurable personal loss and accelerate social and political crises in dozens of countries. In the early 2000s, medicines in the form of combination antiretrovirals (ARV) emerged with the promise of halting the worst effects of the disease and rendering life livable for those infected, but countries struggling under the weight of the epidemic were largely unable to access ARVs due to high costs, low global supply, and patent restrictions. With drug manufacturers worried about profit margins and feeling little incentive to supply infected communities in Africa, reaching the millions infected with these life-saving drugs seemed an impossibility.
The Creation of PEPFAR
The President’s Emergency Plan for AIDS Relief (PEPFAR) was created to meet this global challenge. Conceived as an all-hands-on-deck effort to marshal the resources and momentum needed to halt the crisis of HIV, PEPFAR became the clearest example of positive, forward-looking American leadership in the post-2001 era. US leadership and PEPFAR’s purchasing power pushed drug companies to lower their prices and expand production, while paving the way for more accessible generics. PEPFAR stood up a global infrastructure of collaboration with 14 focus countries—increased to more than two dozen over the years that followed—aimed at expanding testing and rapidly scaling up treatment programs, alongside behavior change and biomedical prevention strategies. With coordinated efforts from the Global Fund for AIDS, Tuberculosis and Malaria (also with critical US support), treatment access expanded from around 50,000 people to more than 20 million between 2004 and 2022.
PEPFAR’s work should not be viewed as purely disinterested, American “do-gooderism.” The long-term and strategic threat caused by disintegrating social and political structures if HIV decimated populations across Africa, eastern Europe and beyond was mitigated in part by PEPFAR and transformed into opportunities for stronger bilateral and multilateral relationships. Against the backdrop of unpopular wars in Iraq and Afghanistan, PEPFAR’s contrasting focus on saving lives was an impactful soft power, “hearts and minds” initiative. Partnerships built through PEPFAR and other US public health programs have built trust and allowed rapid and reliable collaborations to combat other emerging health threats, including Ebola and the recent Marburg outbreaks. Public health diplomacy has long been stressed as a critical weapon in America’s strategic defense arsenal—stronger health systems and partnerships with public health authorities abroad mean more chances to identify and contain emerging outbreaks at their source, and wiser voices than mine have articulated the benefits of PEPFAR to solidify a range of economic, defense and political partnerships.

Yet, when PEPFAR was established, there was also an overtly moral and humanitarian component—whether in response to the lives lost in the quagmire of the Iraq and Afghanistan wars or more broadly in contrast to all the global disasters without clear solutions—here was a situation where we could do something. The framers of PEPFAR—political and public health leaders both—seemingly felt keenly that standing back and doing nothing would be an abdication of America’s values as well as our global leadership. We had a responsibility to act. PEPFAR was bold, groundbreaking and bipartisan when it was created and continues as the exemplar of impactful, innovative global public health collaborations.
PEPFAR marked its twentieth anniversary this year, and despite its remarkable quantitative achievements—more than 25 million lives saved, and more than 65 million people reached with testing and treatment—its real impact has been incalculable. We cannot measure the effects of the deaths which did not occur, communities which did not disappear, or the individual achievements of those who lived. This is, of course, the catch-22 of public health successes—progress is made through disasters averted, when the worst eventuality does not come to pass. Although studies have demonstrated that PEPFAR has been associated with increased GDP and higher rates of schooling for girls in priority countries, for example, it is likely only with the perspective of history that we will really be able to take stock of what PEPFAR has meant writ large.
At a micro-level, the impact is more tangible–I cannot adequately convey the enormity of the crisis facing health personnel in the clinics I visited in Southern Africa, starting in the late 2010s. The scale of the epidemic and its frightening dual burden of tuberculosis was overwhelming health services. Health leaders desperately needed tools, strategies, solutions, resources—just help. Little by little as time went by, I was able to see a difference as testing increased, treatment accelerated, and our conversations shifted from desperate to more calculating as we tried to help leaders push through to reach that last mile of clients and services, with the possibility of bringing the virus under control in sight.
PEPFAR’s Future
So far, six countries have achieved global targets signaling effective control of HIV and more countries are getting closer to that mark, even as new preventive medicines are expanding and progress inches forward on a vaccine. We are not at the finish line—in 2021, an estimated 1.5 million people were newly infected, reflecting progress lost during the COVID-19 pandemic—but as PEPFAR enters its third decade, strategies are rightly shifting from an emergency footing towards enabling countries to design and lead their own responses, in the context of building national health systems. The transition may be awkward at times—PEPFAR has been justifiably criticized over the years for heavy-handedness, dictating to countries how they should run their national programs, and operating parallel health systems. At various times during the program’s existence, US administrations have sought to push countries to take more ownership for HIV, not in a spirit of partnership, but from the standpoint that they should manage “their epidemic” with less money from the US.
I began my public health career in the early days of PEPFAR. Its strategies informed the early HIV projects I supported as a Peace Corps volunteer, which I debated and dissected in graduate school while absorbing the sense of energy and motivation that infused global health during this period. Looking back, it is easy to see how PEPFAR programs, emphasizing scaled-up, data-driven, intensive health center- and community-level work, with flexibility to innovate and embrace new methods have really changed the lexicon of health and development strategies over the last twenty years. I, along with a generation of public health practitioners, absorbed this hands-on, ground-level, across-the-board approach to development, even as I grumbled at the idiosyncrasies of its funding model (of which there are many). PEPFAR has its share of justifiable criticisms—its emphasis on meeting service delivery targets reflects the urgency of the work that needs to be done but can also create perverse incentives and inhibit long-term growth of systems or local partners—though its legacy is still being written.
Our immediate goals shifted somewhat in 2020—as COVID-19 spread, countries in Africa, Latin American and Asia struggled just as we did to balance response options, the need to rapidly expand testing, and keep services going while keeping the public safe. Services and systems built for HIV became a backbone of the COVID response in PEPFAR countries—diagnostic networks and testing platforms supported by PEPFAR were retrofitted for COVID tests, supply chains built around HIV drugs and commodities pushed out COVID supplies to lower-level health centers, and the vast system of surveillance and data reporting required to monitor HIV services helped keep track of how many cases emerged.
PEPFAR has embraced the goal of ending the HIV/AIDS pandemic by 2030, while building on the lessons from COVID to better assist countries to respond to other new and emerging epidemic threats. Whether the world will collectively succeed in ending HIV by 2030 depends on many factors beyond PEPFAR, as it is undoubtedly a tall task, but we can be fairly certain that it won’t happen without ongoing support from the US via PEPFAR and the Global Fund. The ability for public health platforms to sustain societal action to counter epidemic threats is unfortunately not as strong as it should be following COVID, and a number of trends, including the rise of anti-LGBTQ sentiment, faltering progress in countries facing humanitarian crises, and new threats linked to climate change—in short, the combined weight of global polycrises—could derail progress and endanger the lives of people infected with HIV.
PEPFAR has been in the news recently, not to laud its tremendous ongoing impact, but to debate its future. I can’t help but be dismayed by attempts to use PEPFAR to instigate a clash between politics and public health, knowing that the lives and well-being of millions of people are on the line. Failure to continue PEPFAR would immediately imperil individuals, families, communities and societies around the world—and would also needlessly squander the global good will America has won and threaten the social stability we’ve fostered. Attempts to pin unconnected ideological fights onto PEPFAR ignore the fact that PEPFAR is good politics—a historically bipartisan public health initiative that gains us friends and keeps people alive. PEPFAR, with all its faults, is an example of American leadership tackling complex problems, which we should continue to build on.![]()
 For fifteen years, Alisha Smith-Arthur has designed and led public health programs across Southern and West Africa, Eastern Europe and South Asia. Grounded on community and client-focused strategies, she works with governments to address critical infectious disease threats and has extensive experience supporting the expansion of HIV and TB services. As Director of Public Health Preparedness and Global Health Security at RTI International, Alisha focuses on amplifying preparedness platforms for both existing and emerging global pandemic threats, while embracing locally driven solutions and the development of stronger equity, and justice-based models for strengthening health systems to serve the public good. She holds degrees from the London School of Economics and Tulane University and is a returned Peace Corps volunteer from Togo.
For fifteen years, Alisha Smith-Arthur has designed and led public health programs across Southern and West Africa, Eastern Europe and South Asia. Grounded on community and client-focused strategies, she works with governments to address critical infectious disease threats and has extensive experience supporting the expansion of HIV and TB services. As Director of Public Health Preparedness and Global Health Security at RTI International, Alisha focuses on amplifying preparedness platforms for both existing and emerging global pandemic threats, while embracing locally driven solutions and the development of stronger equity, and justice-based models for strengthening health systems to serve the public good. She holds degrees from the London School of Economics and Tulane University and is a returned Peace Corps volunteer from Togo.
